

Looking for low-cost or no-cost health insurance in PA? We offer Medicaid and CHIP plans through the PA Medical Assistance (MA) program. We also offer dual health plans for people with both PA Medicaid and Medicare.
All Pennsylvanians deserve affordable health care. And more people than ever are eligible for no-cost or low-cost health coverage. This includes the seniors, families, people with disabilities, pregnant women and children. You may qualify too.
At UnitedHealthcare Community Plan of Pennsylvania, we’re committed to making a difference in each member’s life. We take great pride in the quality of service we provide to our PA Medicaid and CHIP members. We look forward to serving you.
Whatever plan you choose, UnitedHealthcare will help you get the care you need.
All medicaid and chip members must go through the recertification process annually. It’s not automatic. A renewal form will be sent to you 90 days before your coverage ends. A UnitedHealthcare Community Plan representative may call you to help you with the renewal process. Learn more.
1 Benefits, features, and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply. Other hearing exam providers are available in the UnitedHealthcare network. The plan only covers hearing aids from a UnitedHealthcare Hearing network provider.

Community Plan for Families

Community Plan for Kids

United Dual Complete

As a UnitedHealthcare Pennsylvania Medicaid member, you’ll get extra benefits that some plans don’t offer.
Bucks, Chester, Delaware, Montgomery and Philadelphia

Pennsylvanians on a UnitedHealthcare Dual Special Needs plan (or dual health plan) get many extra benefits beyond those you get with either Original Medicare or PA Medicaid.

CHIP is short for the Children's Health Insurance Program. The CHIP program provides $0 or low cost health insurance to uninsured child and teens, regardless of income status.
With PA CHIP, children get health coverage, including:
Adams, Allegheny, Armstrong, Beaver, Bedford, Berks, Blair, Bradford, Bucks, Butler, Cambria, Carbon, Chester, Clarion, Columbia, Crawford, Cumberland, Dauphin, Delaware, Erie, Fayette, Forest, Franklin, Fulton, Greene, Huntingdon, Indiana, Jefferson, Lackawanna, Lancaster, Lawrence, Lebanon, Lehigh, Luzerne, Mercer, Monroe, Montgomery, Montour, Northampton, Perry, Philadelphia, Pike, Schuylkill, Somerset, Sullivan, Susquehanna, Venango, Warren, Washington, Westmoreland, Wyoming, and York.

Fitness made fun and flexible — in the gym or at home
For UnitedHealthcare Community Plan members over the age of 18, this all-in-one fitness benefit can help you work out when, where and how you want to.

UnitedHealthcare Community Plan covers urgent care. Urgent care is for an illness, injury or condition that, if not treated within 24 hours, could quickly turn into an emergency. It’s when you need to get care from a doctor, but not in the emergency room.
If you have any questions, please call Member Services at 1-800-414-9025, TTY/PA Relay 711.

For members under 21 years of age:
UnitedHealthcare Community Plan provides all medically necessary dental services for children under 21 years of age.* Children can go to any participating dentist in the UnitedHealthcare Community Plan network.
* If braces were placed before age 21, the care will be covered until it is done, or until age 23, whichever comes first. That is, as long as the member remains eligible for Medical Assistance and is still a member of UnitedHealthcare Community Plan.
For members 21 years of age and older:
UnitedHealthcare Community Plan covers some dental services for members 21 years of age and older. Care must be provided by dentists in the UnitedHealthcare Community Plan network. Some dental services have limits. All adult members are eligible for emergency dental services related to treatment for pain.

UnitedHealthcare Community Plan covers family planning services. You don’t need a referral from your primary care provider (PCP). Family planning services include:
You can see any Medical Assistance provider, including an out-of-network provider that offers family planning services.
There’s no copay for covered family planning services.
For more information or to get help finding a family planning provider, call Member Services at 1-800-414-9025, TTY/PA Relay 711.

UnitedHealthcare covers pregnancy care. Prenatal care is the health care women get during pregnancy and through delivery. It could be from a maternity care provider, such as an obstetrician (OB or OB/GYN) or a nurse-midwife.
Early and regular prenatal care is very important for you and your baby’s health. Even if you’ve been pregnant before, it’s important to go to a maternity care provider regularly throughout each pregnancy.
Think you’re pregnant and want a pregnancy test? See your primary care provider (PCP) or a family planning provider.
If you’re pregnant, you can:
Need help finding a maternity care provider? Call Member Services at 1-800-414-9025, TTY/PA Relay 711.

UnitedHealthcare Community Plan covers well child checkups for children under the age of 21. Your child may be seen by a pediatrician (child’s doctor), family practice doctor or nurse practitioner. The provider you choose will be your child’s primary care provider (PCP).
The purpose of well child visits is to make sure children are developing and growing properly and to check for any health problems. Catching physical and behavioral health issues early can make them easier to treat.
If you have questions or want more information, call Member Services at 1-800-414-9025, TTY/PA Relay 711.
Find answers to these health questions and many more.
If you do play video games, play interactive ones where you have to move. You don’t even have to leave the house to move – try exercises like jumping jacks, marching in place, going up and down stairs, push-ups or sit-ups at home.
Walk! Take a walk with a friend outside. Walk your dog or your neighbor’s dog, or walk your cat! Instead of driving, walk or bike to school or a friend’s house.
Clean! Vacuum your room. Wash the car. Mow the lawn. Your parents will be happy, and it’s another chance for you to get more exercise, and maybe even have some fun.
Unplug! Limit your time watching TV or using your smartphone, computer or other device. Keep screen time to less than two hours a day. When you do watch TV or use your phone – try marching in place or exercising while you watch/play.

Our HealthTalk newsletter is now online. The newsletters are a great way to learn about our health plan and important health topics.
You can read it whenever, wherever you want. Check back quarterly for a new edition.
Medicaid Newsletter English | Español
CHIP Newsletter English | Español

PA Medicaid, is health insurance for people with low incomes. You might be able to get Medical Assistance (Medicaid) in Pennsylvania if you’re pregnant, have children or live with a disability. In some cases, other adults may also qualify. Costs to you are low and based on your ability to pay. It’s important to know that Medicaid rules and coverage differ from state to state.
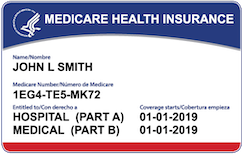
Dual Special Needs Plans (also called dual health plans or D-SNPs for short) are for people who get both PA Medicaid and Medicare. Dual plans cover doctor visits, hospital stays and prescription drugs. They offer more benefits and extras than Original Medicare. You’ll keep all your Pennsylvania Medical Assistance (Medicaid) benefits, too.

CHIP is short for the Children's Health Insurance Program. The CHIP program provides health insurance to uninsured children and teens.
There are a lot of reasons kids might not have health insurance. Maybe a parent lost their job. Maybe their parents don't have health insurance at work. Or maybe it just costs too much. Whatever the reason, CHIP may be able to help.
You might think that your children or teens aren't eligible. A lot of parents are surprised to learn that CHIP can help their families. If you qualify, you can get CHIP at no cost or for a small monthly payment. Either way, no cost or low cost, there are no deductibles.
Disclaimer information (scroll within this box to view)Looking for the federal government’s Medicaid website? Look here at Medicaid.gov.
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. Benefits, features and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Dual Special Needs plans have a $0 premium for members with Extra Help (Low Income Subsidy).
Benefits, features, and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply.
This service should not be used for emergency or urgent care needs. In an emergency, call 911 or go to the nearest emergency room. The information provided through this service is for informational purposes only. The nurses cannot diagnose problems or recommend treatment and are not a substitute for your provider's care. Your health information is kept confidential in accordance with the law. The service is not an insurance program and may be discontinued at any time. Nurse Hotline not for use in emergencies, for informational purposes only.
UnitedHealthcare Connected® for MyCare Ohio (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees.
UnitedHealthcare Connected® (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and Texas Medicaid to provide benefits of both programs to enrollees.
UnitedHealthcare Connected® for One Care (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the member handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® member handbook.
UnitedHealthcare Senior Care Options (SCO) is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare and does not have any other comprehensive health Insurance, except Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our Senior Care Options (SCO) program.
Every year, Medicare evaluates plans based on a 5-Star rating system. The 5-Star rating applies to plan year 2024.
The choice is yours
We will provide you with information to help you make informed choices, such as physicians' and health care professionals' credentials. This information, however, is not an endorsement of a particular physician or health care professional's suitability for your needs.
The providers available through this application may not necessarily reflect the full extent of UnitedHealthcare's network of contracted providers. There may be providers or certain specialties that are not included in this application that are part of our network. If you don't find the provider you are searching for, you may contact the provider directly to verify participation status with UnitedHealthcare's network, or contact Customer Care at the toll-free number shown on your UnitedHealthcare ID card. We also recommend that, prior to seeing any physician, including any specialists, you call the physician's office to verify their participation status and availability.
Some network providers may have been added or removed from our network after this directory was updated. We do not guarantee that each provider is still accepting new members.
Out-of-network/non-contracted providers are under no obligation to treat UnitedHealthcare plan members, except in emergency situations. Please call our customer service number or see your Evidence of Coverage for more information, including the cost- sharing that applies to out-of-network services.
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 ("ADA"), UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
Network providers help you and your covered family members get the care needed. Access to specialists may be coordinated by your primary care physician.
Paper copies of the network provider directory are available at no cost to members by calling the customer service number on the back of your ID card. Non-members may download and print search results from the online directory.
To report incorrect information, email provider_directory_invalid_issues@uhc.com. This email box is for members to report potential inaccuracies for demographic (address, phone, etc.) information in the online or paper directories. Reporting issues via this mail box will result in an outreach to the provider’s office to verify all directory demographic data, which can take approximately 30 days. Individuals can also report potential inaccuracies via phone. UnitedHealthcare Members should call the number on the back of their ID card, and non-UnitedHealthcare members can call 1-888-638-6613 / TTY 711, or use your preferred relay service.
If you’re affected by a disaster or emergency declaration by the President or a governor, or an announcement of a public health emergency by the Secretary of Health and Human Services, there is certain additional support available to you.
If CMS hasn’t provided an end date for the disaster or emergency, plans will resume normal operation 30 days after the initial declaration.